GYNAEC ONCOSURGERY
Gynecologic oncology is a specialized field of medicine that focuses on cancers of the female reproductive system, including ovarian cancer, uterine cancer, vaginal cancer, cervical cancer, and vulvar cancer. As specialists, they have extensive training in the diagnosis and treatment of cancers.
There is low quality evidence which demonstrates women with gynaecological cancer receiving treatment from specialized centres benefit from longer survival than those managed in standard care. A meta analysis of three studies combining over 9000 women, suggested that specialist gynaecological cancer treatment centres may prolong the lives of women with ovarian cancer compared with general or community hospitals. In addition, a meta‐analysis of three other studies which assessed over 50,000 women, found that teaching centres or specialized cancer centres may prolong women's lives compared to those treated in community or general hospitals.
Gynecological cancers comprise 10-15% of women's cancers, mainly affecting women past reproductive age but posing threats to fertility for younger patients. The most common route for treatment is combination therapy, consisting of a mix of both surgical and non-surgical interventions (radiotherapy, chemotherapy).
Signs and symptoms
Signs and symptoms usually vary depending on the type of cancer. The most common symptoms across all gynecological cancers are abnormal vaginal bleeding, vaginal discharge, pelvic pain and urination difficulties.
Ovarian cancer
Bloating or abdominal swelling
Frequent urination
Pelvic or back pain
Increased satiety/loss of appetite
Altered bowel movements
Fatigue
Weight loss
Endometrial cancer
Post-menopausal bleeding
Abnormal vaginal bleeding (heavy or irregular menstrual cycles)
Vaginal discharge
Difficulty urinating
Pelvic pain
Vaginal cancer
Abnormal vaginal bleeding
Vaginal discharge
Pelvic Pain
Painful and frequent urination
Cervical cancer
Abdominal pain
Foul-smelling vaginal discharge
Pelvic pain and/or back pain
Blood spotting
Post-menopausal bleeding
Vulvar cancer
Pruritus: persistent itch in the vulva
Vulvar bleeding
Vulvar pain, soreness or tenderness
Burning sensation when urinating
A visible wart-like mass or sore on the vulva
Types:
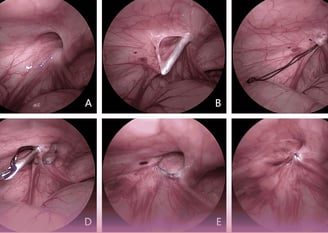
1) Hysteroscopy
A hysteroscopy is a procedure doctors use to diagnose and treat conditions involving the uterus and cervix, such as abnormal uterine bleeding, abnormal endometrial thickening, bleeding after menopause, and infertility.During a hysteroscopy, your doctor inserts a hysteroscope – a thin tube with a light on the end – into your vagina, through your cervix, and into your uterus. They'll be able to see into your cervix and inside your uterus. They can take a sample for later testing if they find anything abnormal.
Hysteroscopy Procedure
You can have a hysteroscopy in a hospital or at your doctor’s office. During the procedure, you may be awake under local or regional anesthesia or asleep under general anesthesia. If you're having general anesthesia, your doctor may ask you not to eat or drink anything for 6 to 12 hours. If you’re awake, your doctor will give you medicine to help you relax. They'll also use medication or tools called dilators to help open your cervix.
Your doctor will likely use a tool called a speculum to keep your vagina open. If you’ve ever had a Pap test, your doctor probably used one during that procedure, too.
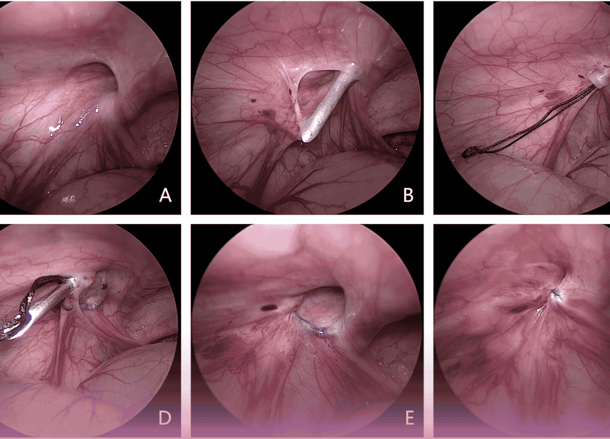
They'll gently insert the hysteroscope through the cervix into your uterus and push gas or a liquid-like saline through the hysteroscope into your uterus to expand it. This will give them a clear view of its lining and the opening of your fallopian tubes.
They’ll then see the insides of your uterus with the images that appear on a video monitor.
If the hysteroscopy is to treat conditions like polyps or fibroids, your doctor will insert the devices for removing the abnormal tissue through the hysteroscope.
The best time to do a hysteroscopy if you have regular periods is the first week after your period ends. You may have a hysteroscopy at any time if you're past menopause. A doctor will not do a hysteroscopy if you:
Are on your period
Are pregnant
Have a pelvic infection
Have genital herpes or signs that you might have it
Have cervical or endometrial cancer
A doctor might also not recommend a hysteroscopy if you have heart disease or tend to bleed easily. Speak with your doctor about any health conditions you might have before a hysteroscopy.
Tell your doctor if you unexpectedly get your period on the week of the procedure. They may need to reschedule it. Also, don’t use vaginal medicines, a douche, or a tampon 24 hours before your procedure.
How long does a hysteroscopy take?
A hysteroscopy usually takes 5 to 30 minutes. In some cases, it can take about an hour. How long the procedure lasts depends on whether you’re having a diagnostic hysteroscopy, an operative hysteroscopy, a diagnostic and operative hysteroscopy, or another surgery with the hysteroscopy.
Is a hysteroscopy painful?
A hysteroscopy can be painful. Pain can sometimes keep a doctor from completing the procedure. But it might also be painless or cause only mild pain. Your pain level depends on whether you were anxious before the procedure, how long it takes, if you’ve ever given birth, and more.
Speak with your doctor about the procedure, your anesthesia options, and medications that may help you feel calm.
2)Lap Hysterectomy:
A hysterectomy is a procedure to remove your womb (uterus). The neck of your uterus (your cervix) is usually also removed. Your ovaries may need to be removed at the same time.
What are the benefits?
There are common reasons for having a hysterectomy:
Heavy or painful periods not controlled by other treatments.
Fibroids, where the muscle of your uterus becomes overgrown.
A hysterectomy may cure or improve your symptoms. You will no longer have periods.
What does the procedure involve?
The procedure is usually performed under a general anaesthetic but various anaesthetic techniques are possible. The procedure usually takes about 90 minutes.
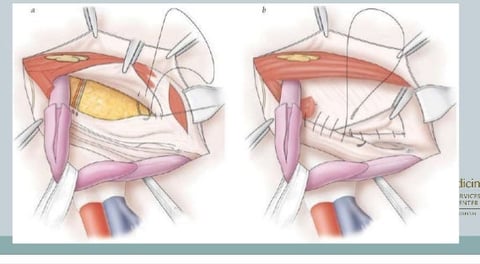
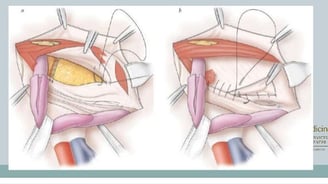
Your gynaecologist will make a small cut, usually on or near your belly button, so they can insert an instrument in your abdominal cavity to inflate it with gas (carbon dioxide). They will make several small cuts on your abdomen so they can insert tubes (ports) into your abdomen. Your gynaecologist will insert surgical instruments through the ports along with a telescope so they can see inside your abdomen and perform the procedure.
Your gynaecologist may need to place instruments through your vagina to help them remove your uterus.
They will make a cut around your cervix at the top of your vagina so they can remove your uterus and cervix.
3)Robotic radical hysterectomy:
A robotic-assisted hysterectomy is a type of hysterectomy your surgeon performs with the help of a robotic machine. Hysterectomy is a surgical procedure to remove your uterus. Your uterus is a hollow, muscular organ in your pelvis. It’s where a fetus grows during pregnancy.
In this type of hysterectomy, your surgeon makes small incisions (cuts) in your abdomen and uses robotic arms to separate your uterus from its surroundings. A robotic hysterectomy is different from a traditional hysterectomy because a surgeon controls the robotic arms with a controller while looking at a screen instead of being over top of your body. The surgeon has complete control over the robotic arms at all times.
There are several methods your surgeon may use to perform a hysterectomy. A robotic hysterectomy is just one of a few methods they may suggest based on your health history and diagnosis. It’s a type of minimally invasive surgery, which means surgery through small incisions.
People who have robotic-assisted hysterectomy often experience less pain, less blood loss and faster recoveries when compared to an open abdominal hysterectomy. Surgeons perform robotic hysterectomy using a da Vinci surgical system. This tool helps surgeons perform a variety of other minimally invasive surgeries.
Why do surgeons use robotic-assisted hysterectomy?
Some of the benefits a robotic-assisted surgery gives your surgeon are:
A 3D, high-definition view of the surgical field with up to 15 times the magnification.
Instruments that mimic the movement of human hands, wrists and fingers, allowing an extensive range of motion that’s more precise than natural hand and wrist movements.
A constant steadiness of the robot arms, fingers and wrists make it easier to operate on organs and tissues for long periods of time and from angles and positions that are typically hard to reach.
Why would someone need a robotic hysterectomy?
Robotic hysterectomy is not for everyone. You and your surgeon will discuss if robotic-assisted surgery is possible and appropriate for you. This type of hysterectomy may be especially helpful if you have obesity or a complex surgical case, such as pelvic adhesive disease (scar tissue that binds nearby organs together).
A hysterectomy treats several conditions. Your healthcare provider may recommend it if you have conditions like:
Abnormal or heavy vaginal bleeding.
Severe and chronic pelvic pain.
Uterine fibroids.
Uterine cancer.
Uterine prolapse.
Advanced stage endometriosis.
Procedure Details
What happens in robotic-assisted hysterectomy?
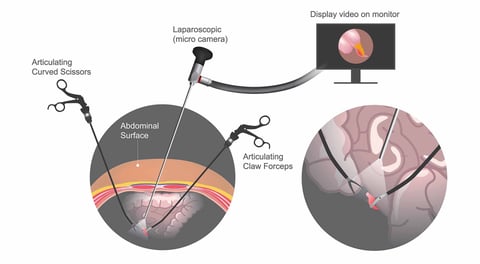
Robotic-assisted hysterectomy is a type of laparoscopic surgery. Laparoscopic surgery is less invasive than traditional surgery. Your surgeon makes several small cuts (less than or equal to 1 centimeter long) on your abdomen, then inserts a laparoscope and other surgical instruments through the incisions. A laparoscope is a thin tube with a light and video camera at the end.
The laparoscope projects the scene of the surgery onto a high-definition video screen. Your surgeon watches the screen to perform the surgery. Robotic-assisted surgery means they control the surgical instruments using robotic arms, while sitting at a computer console a few feet away.




Care
Committed to excellence in patient healthcare services.
Health
Trust
contact@gvkprimeclinics.com
Digibrainz © 2024. All rights reserved.
